
You may begin drinking the day of surgery. You will start on a bland liquid diet such as Gatorade, tea, coffee, water, soup and crackers, or jell-o. You will continue this clear liquid diet for the first 1-2 days post-op. If you are doing well, you will then be advanced to a full semiliquid diet, consisting of foods such as milkshakes, puddings, and soups. Continue this diet for another 3-4 days. If you are still doing well, you should advance to easy-to-swallow soft foods for a period of 2-3 weeks. Hard foods, such as raw vegetables, hard meat, and crusty bread, are avoided until you are completely healed from the operation. Most people can eat a regular diet by 3-4 weeks after the surgery.
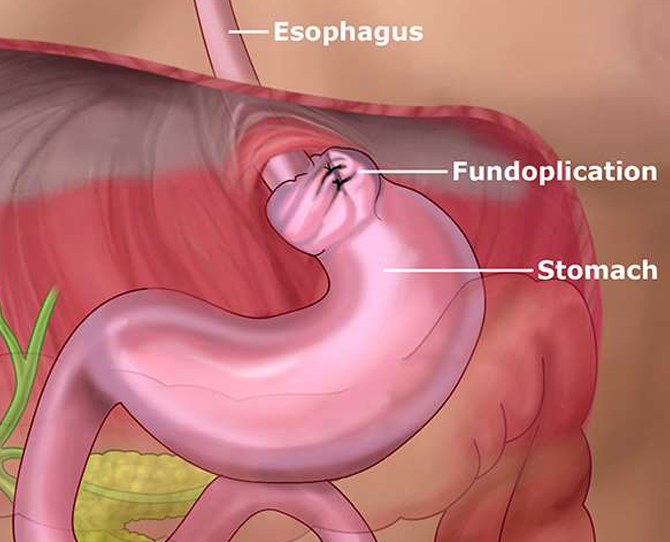
Abdominal cramping and flatulence, caused by increased air in the gut, may occur. Swallowed air may accumulate because the valve is tight. Cramping usually eases in a few months, but flatulence may be permanent. Another common postoperative occurrence is feeling full very quickly (called early satiety) during meals, sometimes just after a few bites. This is because the stomach may have been made smaller. Initially, patients are advised to eat and drink several small meals throughout the day to avoid overtaxing the digestive tract and make sure they are getting adequate nutrition. Over time, the stomach adjusts to accommodate a normal meal.
As soon as you reach home, you may resume normal ad lib activity. You are encouraged to begin walking and resuming household activity as tolerated immediately. Going up and down stairs is also Ok. You should refrain from engaging in any strenuous activity such as running, riding a bike, heavy exercising in a gym, etc. for at least 6 weeks. You should also avoid any heavy lifting greater than 10-15 lbs. for 6 weeks. After that, you may usually resume any activity as tolerated. Avoid any activity that may cause a significant increase in your intra-abdominal pressure for at least 6 weeks after the surgery.
You will most likely have Band-Aids on your incisions. Leave these on for 24 hours after the surgery. You may remove the outer bandage any time after 24 hours, but try not to remove the bandage any earlier than 24 hours post-op. You may have steri-strips on your skin over the incision and underneath the bandage. If so, leave these on for 1 week and then remove and leave off. The incision will most likely be closed with dissolvable sutures that are underneath the skin.
You do not need to do anything about these, and they will never need to be cut out or removed. They will dissolve on their own eventually. You may shower starting 24 hours after the surgery. Running soap and clean water over the incision is Ok but avoid submersing the incision in any dirty water such as baths, lakes, swimming pools, jacuzzies, etc. for at least 2-3 weeks. You may apply ice to the wound for 15–30-minute intervals at a time for pain or swelling, for several days after the surgery. A small amount of bleeding, redness, and swelling may be normal. If there is any excessive pain, bleeding, swelling, redness around the wound, green/white drainage, or fever, please call your surgeon immediately.
You may resume all your normal medications after surgery except for any anticoagulants. You should wait at least 48 hours after surgery before beginning your anticoagulants, as long as there are no signs of external bleeding or bruising. You may need to wait longer, but please consult your surgeon first.
You will most likely be sent home with a prescription for narcotic pain medications. Use the narcotics as directed on the prescription. You may take less than what is indicated on the bottle, but not more. Be sure to take narcotic pain medication with food so as not to upset your stomach. You may begin to taper your narcotic medication as tolerated and discontinue them as soon as possible. As you are tapering off the narcotics, you may transition over to Ibuprofen. You should not drive or operate any mechanical equipment while on narcotic medications. Wait for at least 24 hours after discontinuing the narcotic medications before driving.
It is not unusual for patients who have been through surgery, a general anesthesia, and who are taking narcotics to become constipated. This can often be remedied by increasing your activity and making sure you stay hydrated. In addition, you should also increase your fiber intake in your diet and through supplements (Metamucil, Benefiber, etc.). While on the narcotics, you should also try to take an over-the-counter stool softener such as Colace or Senokot. You should have a bowel movement every day but may go 2-3 days after surgery without one. If you have not had one by two days after surgery, or every 1-2 days afterwards, you may need to try an over-the-counter laxative such as MiraLAX or Magnesium Citrate. If none of these measures work or if you begin to have significant abdominal pain, nausea/vomiting, or diarrhea, please contact your surgeon immediately.
You will be instructed as to when you should return to the office on your discharge instructions. You should call the office to schedule this. You will usually be seen again approximately 2-3 weeks after the surgery.